[ad_1]
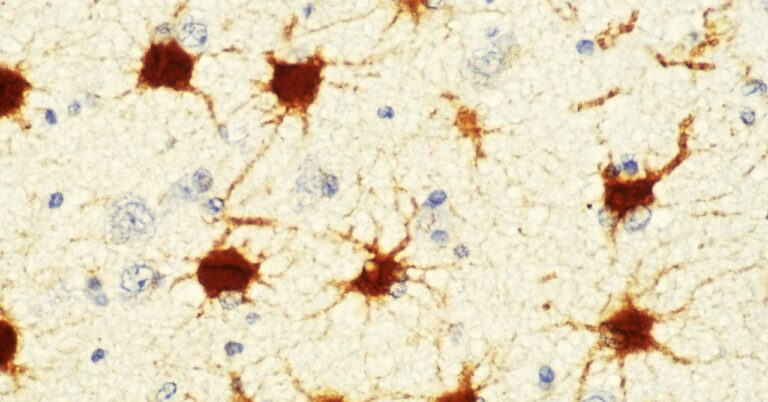
This was slow going. “We spent a lot of time, probably the first couple of years, really just working out the immunopanning and culturing the astrocytes,” recalls Caldwell. One challenge was making sure that the media contained few proteins to start with—those would have interfered with their measurements. The scientists also needed to make sure that culturing the astrocytes in a petri dish would not change their behavior from how they would have acted in the brain.
Once they’d established that the cultured cells behaved normally and maintained their ability to direct neuronal development, the scientists looked at the proteins they made and the genes they expressed. Then they compared those to normal cells. Across all three disorder models, they found 88 proteins, and approximately 11 genes, that were upregulated—meaning their quantity or expression increased.
Both Caldwell and Allen were surprised that the two were often out of sync. While one might think that an increase in a gene’s expression would correlate with an increase in the protein associated with it, this wasn’t exactly the case. Across the three disorders, there wasn’t much overlap between the genes that were most overexpressed and the proteins that were most overproduced. “I think it really highlights, particularly for different disorders, that you’ve really got to look at protein,” Allen says, rather than focusing on gene expression alone.
Baldwin, who was not involved in the study, concurs—noting that this lack of overlap is a “striking” result. “What sequencing can’t capture, that proteomics can, is all the regulation that occurs when the protein is produced,” she says. Sequencing tells you which gene transcripts are available, she adds, but “doesn’t necessarily tell you which ones are being turned into protein, or at what rate they are being turned into protein.”
Allen’s team focused on a few particular proteins that had spiked across all three disorder models. One is called Igfbp2, which inhibits the gene pathway for insulin-like growth factor (IGF)—a hormone that normally aids in brain development. “The idea was that there was too much of this inhibitor being made by the astrocytes,” says Allen. So the lab tried suppressing it. They gave living mice with Rett’s syndrome an antibody that blocked Igfbp2, and they found that their neurons grew more normally.
Another protein that was overproduced in all three animal models is called Bmp6. It’s thought to regulate astrocyte maturation. Again, the team tested what happened when they turned the protein down. First, they placed mouse neurons in a dish, then added the proteins secreted by astrocytes from mice with Fragile X. The neurons weren’t able to grow many neurite tendrils. But when the scientists tried again, this time with the ooze from Fragile X astrocytes treated with a Bmp6 inhibitor, those tendrils grew. Knocking out production of the Bmp6 protein seemed to lead to more normal neuron development.
And as it turns out, the two proteins may be interconnected—turning up Bmp6 may also turn up Igfbp2, Allen says, “and that is leading to some of these deficits.”
[ad_2]