Inside a two-story brick building, not far from the orchids and iguanas of the botanical garden in Medellín, Colombia, wildlife technician Jorge Asprilla demonstrates how to extract venom from a snake. First, he uses a metal hook with an extended handle to snag a five-foot-long pit viper. Then he has to grab its head without getting bitten—a skill he has perfected after working for more than 25 years with dozens of venomous snake species.
Soon Asprilla has the snake’s spade-shaped head firmly in his grasp and its muscular body pinned between his legs. The snake in his grip is known locally as a mapaná, and this species is responsible for most of the snakebites in Colombia. Asprilla has been bitten twice since he started working at the University of Antioquia’s serpentarium, but he isn’t one to elaborate on the experience. “Duele mucho,” he says. (“It hurts a lot.”)
Venomous snakes bite about 5,000 people a year in Colombia; between 20 and 40 of those bitten die from their injuries. And although Colombia has the ability to produce and distribute antivenom—the antidote for venomous snakebites—about 20 percent of the victims who need antivenom don’t receive it. Globally as many as 2.7 million people are envenomed by snakes every year. Of these, up to 400,000 are permanently disabled, and estimates suggest that 81,000 to 138,000 die. Venomous snakebites may receive less attention from health organizations than contagious viruses and bacterial infections, but their toxic effects make them one of the deadliest neglected tropical diseases.
Asprilla moves the hook into the mapaná’s mouth, just behind its pallid, curved fangs. As he massages the snake’s head with his hand, a bead of gold venom oozes out of a tooth. This liquid is responsible for both life and death: it can kill a human in days, and it can be used to produce the antivenom that might save someone by counteracting a venomous bite. Despite the existence of such antivenom, however, people continue to die. Asprilla’s work is part of a project aiming to change that.
Snakebites aren’t limited to low-income countries. Australia, for instance, has more venomous snakes than nonvenomous ones. But because of lifestyle factors and access to health care, the country records relatively few deaths from snakebites every year. In many low-income nations, dangerous bites are a pervasive threat. Most people bitten by snakes live in poverty, many of them in rural areas far from good medical care. They are rice farmers who tend to their fields in bare feet, herders who walk their cattle in the bush, families who sleep on the floor in homes with abundant entry points for snakes and the rodents they feed on.
“These people, these farmers, are voiceless. They don’t have any good representation,” says Abdulrazaq Habib, an infectious and tropical disease doctor at Bayero University in Kano, Nigeria. For many victims, antivenom comes too late or not at all.
Exactly how many people are bitten, and how many of those people die, is difficult to determine. Official records often underestimate the incidence. Victims might die before they reach the clinic, or they might seek care from a traditional healer. Even those who do go to the doctor might not be counted. In many countries, doctors aren’t obligated to report snakebites to the government. Estimates based on household surveys aren’t always accurate, either. What is clear is that India and Pakistan bear the brunt of the impact. According to one estimate, in 2019 more than 75 percent of the people who died from snakebites globally were residents of those countries. In India, venomous snakes kill some 50,000 people a year. In the U.S., although 7,000 or 8,000 people are bitten by venomous snakes every year, about five of them die.
The World Health Organization, under pressure from some of its member states, added snakebite envenoming to its list of neglected tropical diseases in 2017 and, two years later, laid out a strategy for prevention and control. The organization aims to halve the number of deaths and cases of disability by 2030. But the world has made little progress toward that goal, which many experts believe is unrealistic.
On the surface, reducing snakebite deaths seems easy, says David Williams, a toxinologist who assesses antivenoms for the WHO. Dig a bit deeper, however, and the true complexity of the problem emerges. Not every country has the same variety of venomous snakes. Species with different toxins require different antivenoms. The world produces less antivenom than it needs, and production quality varies. The cost to manufacture the remedy is more than most patients can afford. And those bitten often live in remote areas where they can’t access antivenom quickly.
The most intractable obstacle, however, is apathy. Snakebite envenomings are “the most neglected among the neglected,” says snakebite expert Mohammad Abul Faiz, a retired physician and current president of the Toxicology Society of Bangladesh. Few politicians seem to care about solving the problem.
Ending the snakebite crisis will require education, cooperation, research and, most of all, money. Countries need to make the problem a priority, Williams says: “If they choose not to invest in [the problem], then, to be perfectly honest, it doesn’t matter what the rest of us do. We will never change anything.”
Production Woes
Antivenom production today is a modernized version of a technique first used 120 years ago. Technicians inject minuscule quantities of venom into horses or sheep over several weeks, then harvest their blood and extract the antibodies—all of them. In most cases, Williams says, “What you’re getting in the vial is not just antibodies that are specific to the venom of the snake but antibodies for all the other antigens that horse was ever exposed to.”
Once the antivenom gets injected into a patient, some of those antibodies will bind to the various components of the snake venom and neutralize it. Because different kinds of snakes carry different toxins, the antivenom typically must match the species. The approach prevents venom from causing damage, but it can’t reverse damage that has already been done, so it works best in the first couple of hours after the bite. That means a person must reach a treatment facility quickly, the facility must have the appropriate antivenom in stock, and a doctor must administer it. The system is labor-intensive, inefficient and littered with obstacles.
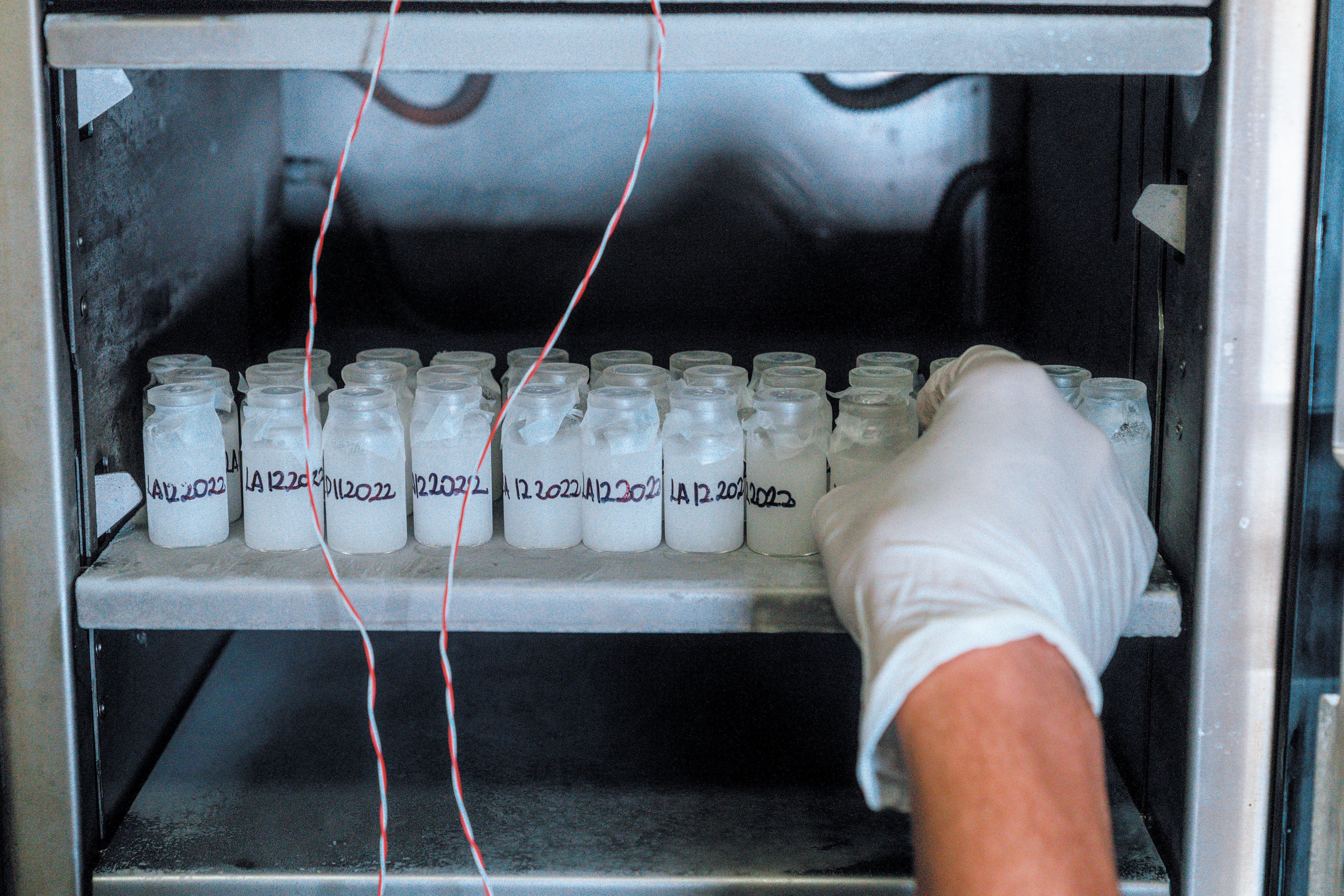
Antivenom production in Colombia has dwindled in recent years from three sources down to one. Colombia’s National Institute of Health produces about 10,000 to 20,000 vials a year. That’s not enough, according to calculations by Sebastián Estrada-Gómez, a toxinologist at the University of Antioquia who helped to create the antivenom company Tech Life Saving, a spin-off of the university and part of a biotech development firm called Tech Innovation Group. With help from an angel investor, Estrada-Gómez has started to produce antivenom just outside Medellín with his “crew”: Diabla, Elisa, Margara, and more than a dozen other sleek, brown and white horses that are part of his antivenom production. The government provides liquid antivenom, but Estrada-Gómez is working to make a freeze-dried product that doesn’t require refrigeration and has a longer shelf life.
Think Local
Sri Lanka, an island nation slightly larger than West Virginia, is home to about 100 species of snakes, roughly a quarter of which are venomous. Experts estimate that as many as 60,000 people there are bitten by venomous snakes every year, and 200 of those people die. The country gets nearly all its antivenom from India, the largest producer and exporter of antivenom in the world.
Indian antivenom targets the “big four” species of venomous snakes in the region: the Indian cobra, the common krait, Russell’s viper and the saw-scaled viper. These four species account for most of the venomous snakebites in India. Sri Lanka also is home to all these snakes, but its most frequent envenoming is from the hump-nosed pit viper, for which no commercially available antivenom exists. Although its bites are rarely fatal, they can cause excruciating pain and swelling. In some cases, they can lead to kidney damage. Tissue death around the bite may require skin grafts or amputation. The bites are most severe in small children.
Complicating the problem even further, antivenom against the same species may not work equally well in different locales. Some evidence suggests that antivenom developed using venom from Indian Russell’s vipers, for instance, is less effective against venom from Sri Lankan Russell’s vipers.
In an ideal world, Sri Lanka would make its own antivenom. About a decade ago collaborators from the U.S., Costa Rica and Sri Lanka formed a partnership to do just that. A U.S.-based nonprofit called Animal Venom Research International helped to set up Sri Lanka’s first serpentarium and train staff to extract venom. Sri Lankan technicians collected the venom and shipped it to the Clodomiro Picado Institute in Costa Rica, one of the premier antivenom production facilities in the world. The institute produced more than 3,000 vials of antivenom targeting five species, including the hump-nosed pit viper. Researchers at the University of Peradeniya in Sri Lanka then used those vials to launch a clinical trial. The trials are ongoing, and no results have been published.
But Kalana Maduwage, a physician and antivenom researcher who was part of the project, says that data showed just a single vial of the antivenom can neutralize hump-nosed viper bites. For Russell’s viper bites, the antivenom seems to produce fewer allergic reactions than other available options.
The ultimate goal was to transfer the technology from Costa Rica to Sri Lanka. Maduwage even trained in Costa Rica to learn how to produce the antivenom. But when he got back to Sri Lanka, he and his colleagues couldn’t get funding to push the project forward. The serpentarium still exists, and Maduwage, who is now based at the University of New England in Armidale, Australia, says the Sri Lankan government is willing to buy the antivenom if the country can produce it. But the team needs at least $10 million to build the production facility. He understands why investors might be hesitant. Antivenom is expensive to produce, and demand in Sri Lanka is limited, so it could take years to turn a profit, Maduwage says. “This is not an easy money-making project.”
The lack of profitability is an obstacle not just in Sri Lanka but worldwide, says José María Gutiérrez Gutiérrez, a toxinologist and former director of the Clodomiro Picado Research Institute. The problem might be one that the market alone can’t solve. Rather he says there needs to be greater involvement by the public sector, an approach that has worked well in Costa Rica. The Clodomiro Picado Institute, which is publicly funded, not only provides enough antivenom to meet Costa Rica’s needs but also ships antivenom throughout Central America as well as to countries in South America and sub-Saharan Africa. The country has an abundance of venomous snakes but has managed to keep snakebite deaths low, with three or fewer a year.
Costly Cure
Bolstering antivenom production will address only part of the problem. The remedy must be not just accessible but affordable. It is often neither. In Nigeria, for example, a small and bad-tempered snake called the West African carpet viper is responsible for most of the country’s bites. The government supplies antivenom free of cost, but there is not enough to help everyone in need. In 2017 the Nigerian government spent only $192,000 on its antivenom program, which is enough money to treat about 4 percent of the country’s snakebites. To halve the number of deaths, as the WHO hopes to do, Nigeria would have to spend about 50 times that amount.
When free antivenom is not available, the cost to individuals can be prohibitive. The therapy runs anywhere from $60 to $150 per vial, and a patient might need more than one. Yet 40 percent of the Nigerian population makes less than $2 a day. Antivenom, Habib says, “is a catastrophic health expenditure.” On top of that, patients must also cover the high cost of bite-associated injuries, which have to be treated at a hospital. Because carpet viper bites cause bleeding and tissue decay, some victims may need blood transfusions. Unluckier ones may need dead tissue sliced out of their wound or a limb amputated.
Because hospital costs are so high, many people try to avoid hospitals altogether. “Victims visit traditional healers first,” Habib says. “It’s cheaper and probably more accessible.” It’s also ineffective. The therapies these healers provide—sucking venom from the wound, applying tourniquets and offering charred animal bones called “black stones”—not only delay access to care but also can lead to additional medical complications.
Even when antivenom is accessible, obstacles persist. The therapy can cause life-threatening anaphylaxis or other allergic reactions because of horse proteins in the antivenom or contamination during production. The risk of a reaction can be 40 percent or more depending on the patient’s susceptibility, the number of vials administered and the purity of the antivenom. In serious cases, doctors might have to provide adrenaline to counteract the reaction or even intubate the patient. When hospitals aren’t properly equipped to deal with these complications, antivenom can kill.
Worries over these outcomes have made some doctors and nurses too nervous to use antivenom therapies. Ravikar Ralph, a physician at the Christian Medical College in Vellore, India, says that snakebite patients often travel from a remote area to their closest medical center for treatment. But given all the potential complications, it’s not uncommon for physicians in these small clinics to doubt their ability to treat a snakebite and send patients to a larger hospital. One survey found that only a third of Indian health-care professionals knew how to correctly manage adverse reactions to antivenom. “Invariably what happens is that these patients are then sent off to larger hospitals,” Ralph says. The resulting delay in treatment can be a matter of life or death.
The health-care workers’ lack of trust in antivenom spills over into the general public. “If you invite the community to come to the hospital and you are not able to provide services, then why will they come?” Faiz says.
This fear and mistrust can be countered with education campaigns. When snakebite cases ballooned in Baringo County, Kenya, in 2018, Doctors Without Borders stepped in. The organization helped to train 200 health-care workers to manage snakebites and taught community members how to avoid bites and provide first aid for victims. Julien Potet, an adviser on policy for neglected tropical diseases at Doctors Without Borders in Paris, says that training, combined with better antivenom access, made a significant difference in Baringo County. It’s only one example, Potet says, but it shows what is possible.
New Advances
Snakebite envenomation may be one of the most neglected tropical diseases, but a growing number of people are paying attention and working from all angles to try to improve patients’ outcomes. A variety of tools are moving forward, from tests to detect venom in the blood, to antivenoms that are easier to produce, to oral medications that could help even before victims arrive at the hospital.
In Sri Lanka, delayed care isn’t a result of transportation difficulties or avoidance by doctors—people who have been bitten typically make it to the hospital within an hour. Once there, however, the country’s snakebite management guidelines advise physicians to wait for a patient to develop signs of systemic envenoming, such as bleeding or kidney failure, to avoid causing unnecessary side effects in case the snake was not venomous or didn’t release any venom. (For some species of venomous snakes, roughly half of bites are “dry” bites with no venom.) “By the time the patient develops clinical features, organ damage has already started,” Maduwage says. That’s why he started working on a rapid bedside test to detect snake venom in blood. “I know how to develop this point-of-care device. I have the technology,” he says. “It was hindered by finances and funding.”
Researchers are also working on better antidotes. Snake venom consists of a complex concoction of toxins, made from dozens of different proteins and peptides. Monoclonal antibodies, which are lab-made antibodies produced in human cells, could be manufactured faster than antivenoms—in days instead of months—and could avoid some of the allergic reactions they cause. But monoclonal treatments are also pricey, and different combinations of antibodies would still be required for each snake species.

Ophirex, a California-based biotech company, aims to eliminate that problem and is pursuing a near-universal therapy. Because snake venom is such a motley combination of molecules, Ophirex is targeting what seems to be a common component: an enzyme called secretory phospholipase A2 (sPLA2) that occurs in 95 percent of snake venoms. In 2021 the company began a randomized, double-blinded, placebo-controlled study—the gold standard of clinical trials—to evaluate the safety and efficacy of its drug varespladib in people who had been bitten by venomous snakes. If it works, the therapy won’t be a panacea, but it might buy people time to reach the hospital, Potet says.
These therapies will be valuable tools if they prove safe and effective, but approval is probably years away. “I’ve been hearing people talk about a universal antivenom for decades,” the WHO’s Williams says, adding that the process takes an inordinate amount of time. “We’re still waiting to see it happen.” Ideally, he would like to see more money and energy spent on improving existing antivenom production to enhance potency and safety. Jean-Philippe Chippaux, an expert on snakebites and former director of research at the French National Research Institute for Sustainable Development, agrees. Even if new drugs existed, hospitals would have to stock them, physicians would have to be trained to use them, and patients would have to be able to afford them, Chippaux says. “I don’t mind researchers experimenting with new, shiny tools as long as they don’t suck all the money out of the field,” he adds.
In theory, reducing snakebite deaths—even by the amount suggested by the WHO—is not impossible. Better antivenoms combined with community education, additional training for health-care workers and accessible medical care could save lives now. “In Bangladesh, in some hospitals the mortality is zero. So this is possible,” Faiz says.
Even the best treatments, however, cannot begin to get at the root problem: poverty. “Neglected tropical diseases, by definition, thrive in rural settings or in disadvantaged communities,” Potet says. “And snakebite is not an exception to that rule.”
Preventing snakebites requires improving access to water, creating indoor toilets, using beds with netting, installing lighting and changing farming practices. Preventing deaths and chronic injury requires overall strengthening of the health-care system. “Until you do this and improve the social and economic status of those vulnerable sections of community, you really will not be able to tackle the problem of snakebites,” Ralph says.
Back in the small brick building in Medellín, Asprilla returns the snake to its home, a glass vivarium that stretches from floor to ceiling. There are five snakes behind the glass, he says, although only three are noticeable.
“That’s how the accidents happen—you don’t see the snakes,” Estrada-Gómez says. He has worked at the serpentarium with Asprilla for nearly two decades, but he’s still reluctant to extract venom from snakes. The one closest to the door has wound its body into a series of S-shaped bends. “He’s trying to accumulate energy to strike.”
Estrada-Gómez finds working with horses much more rewarding. Most of the venom from the serpentarium goes to antivenom production at the farm near Medellín’s airport where he works. His goal is to make sure Colombia has enough antivenom to go around. He can’t solve every problem, but he can try to do something about this one.
“If you have a therapy that you know can work, and it can save lives, and you can produce it, why are people dying?” he says. “It’s unbelievable that still people are dying.”
This article is part of “Innovations In: Environmental Health Equity,” an editorially independent special report that was produced with financial support from Takeda Pharmaceuticals.


