In a new step for Crispr, scientists have used the gene-editing tool to make personalized modifications to cancer patients’ immune cells to supercharge them against their tumors. In a small study published today in the journal Nature, a US team showed that the approach was feasible and safe, but was successful only in a handful of patients.
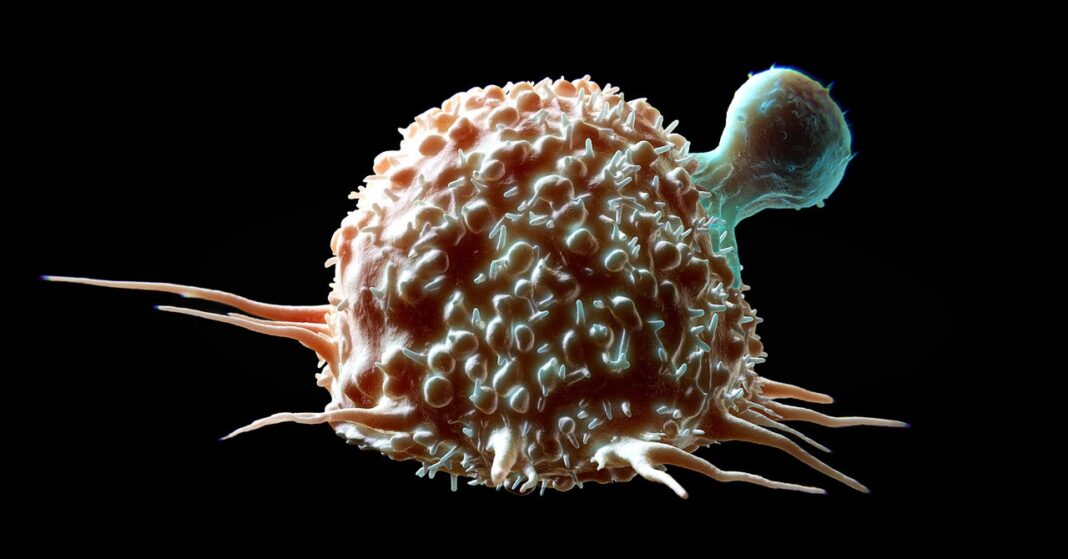
Cancer arises when cells acquire genetic mutations and divide uncontrollably. Every cancer is driven by a unique set of mutations, and each person has immune cells with receptors that can recognize these mutations and differentiate cancer cells from normal ones. But patients don’t often have enough immune cells with these receptors in order to mount an effective response against their cancer. In this Phase 1 trial, researchers identified each patient’s receptors, inserted them into immune cells lacking them, and grew more of these modified cells. Then, the bolstered immune cells were unleashed into each patient’s bloodstream to attack their tumor.
“What we’re trying to do is really harness every patient’s tumor-specific mutations,” says Stefanie Mandl, chief scientific officer at Pact Pharma and an author on the study. The company worked with experts from the University of California, Los Angeles, the California Institute of Technology, and the nonprofit Institute for Systems Biology in Seattle to design the personalized therapies.
The researchers began by separating T cells from the blood of 16 patients with solid tumors, including colon, breast, or lung cancer. (T cells are the immune system component with these receptors.) For each patient, they identified dozens of receptors capable of binding to cancer cells taken from their own tumors. The team chose up to three receptors for each patient, and using Crispr, added the genes for these receptors to the person’s T cells in the lab.
Scientists grew more of the edited cells, enough to constitute what they hoped would be a therapeutic dose. Then they infused the edited cells back into each of the volunteers, who had all previously been treated with several rounds of chemotherapy. The edited T cells traveled to the tumors and infiltrated them.
In six of the patients, the experimental therapy froze the growth of the tumors. In the other 11 people, their cancer advanced. Two had side effects related to the edited T cell therapy—one had fevers and chills, and the other one experienced confusion. Everyone in the trial had expected side effects from the chemotherapy.
Mandl suspects the response to the therapy was limited because the patients’ cancers were already very advanced by the time they enrolled in the trial. Also, later tests revealed that some of the receptors the team chose could find the tumor, but didn’t have potent anticancer effects.
Bruce Levine, a professor of cancer gene therapy at the University of Pennsylvania, says the ability to rapidly identify patients’ unique cancer receptors and generate tailored treatments using them is impressive. But the challenge will be in picking the right ones that actually kill cancer cells. “The fact that you can get those T cells into a tumor is one thing. But if they get there and don’t do anything, that’s disappointing,” he says.